
Septal Perforation
Septal perforation, is a term used to describe a hole or opening within the nasal septum. While some septal perforations can be asymptomatic, some can create issues including nasal obstruction, crusting, pain, and epistaxis.
There are many cause of septal perforation:
- Septal surgery
- Septal hematoma
- Cocaine
- Intranasal drug use
- Infection
- Autoimmune Disorders
- Nose picking
- Violent nose blowing
- Nasal sprays
Treatment
Treating a septal perforation is tailored to the patient. In some patients who are asymptomatic, or the perforation is posteriorly located medical treatment with nasal saline, gels can be helpful. In patients with extremely large perforations, closure may not be possible and supportive treatments to such as salines and gels can be helpful.
Smaller perforations may be able to be treated with an endonasal approach. The tissue is recruited locally and then closed. Often times a spacer of fascia is helpful to ensure closure.
Medium sized perforations can be closed by a few methods. An inferior turbinate flap is usually reserved for small to medium sized perforations. It involves creating a flap based on the tissue surrounding the turbinate and using this to close the defect. The main issue with this flap is that it has a limited reach and application for perforations. Local advancement flaps from either the top of the nose or the floor of the nose are used for small, medium, and large sized perforations. This requires an open approach to the nose. The flaps are recruited from the top or floor of the nose and the closed without tension.
Larger size perforations which are symptomatic can be closed with using local tissues and advancing them. The advantage of locally based flaps is that the blood supply, which can be compromised in a patient with a septal perforation, is not as much of an issue. Finally, free flaps (a transfer of tissue from one are to the nose and connected with blood vessels) is another option. This technique is typically reserved only for the largest of septal perforations.
Principle of Closure:
- Good blood supply to the area
- Mucosa well nourished and not overly dry
- No tension on surrounding area
- Consider spacer if using surrounding mucosa
The main principle of septal perforation is to ensure a good blood supply to the area. Techniques such as skin grafting will often fail as the graft will not have enough blood supply to survive. The blood supply either from the inside of the nose or from a surrounding area can be assessed to see what tissue will provide the best chance of closure.
Prior to septal perforation closure, the patient should hydrate the nose with nasal saline and nasal oil if applicable. This is good advice not only for patients with septal perforation but with patients of dryness of any kind. While nasal dryness is a fairly common symptom in many patients without septal perforation, it can be seen more readily in patients with septal perforation.
When closing a septal perforation, closure to the surrounding tissues must not have tension. The analogy here is imagining lifting a wet tissue paper and trying to first lift this and connect it to another piece of tissue paper. Any tears in the paper will result in likely failure of the septal perforation closure.
Spacers have been shown in several studies to help closure rates. It is important to note, this is in studies using conventional techniques typically rearranging the tissue (sliding it in the nose). The spacer, which can be either cartilage, fascia or PDS plate, allows the surgeon the chance to place the graft in between the flaps and provide a background to close to. Less conventional techniques do not require a tissue spacer.
Large Septal Perforation Closure Technique
 Septal Perforation Septum
Septal Perforation Septum
In the past, septal perforation has been one of the more difficult techniques to master. Most surgeons utilize a sliding technique approach. However, the main weakness of this approach is limited by the amount of surrounding tissue in the nose. In some cases, even with use of nasal saline and other techniques to improve the surrounding mucosal lining of the nose, the surrounding mucosa is too damaged to be used to close the perforation.
 Septal Perforation Pericranium
Septal Perforation Pericranium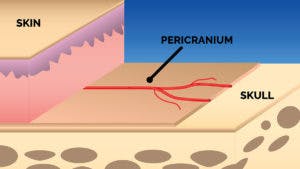 Septal Perforation Pericranium
Septal Perforation Pericranium Septal Perforation Endoscopic
Septal Perforation Endoscopic
Dr. Shah utilizes a specialized approach to septal perforations where he takes the pericranium, or the lining of the skull, and through an endoscopic incision, uses a vascularized flap to close the perforation.
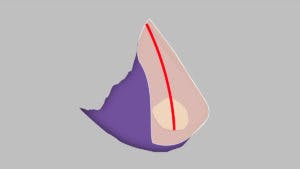
 Septal Perforation Fold
Septal Perforation Fold Septal Perforation Cover
Septal Perforation Cover
The flap is then folded into the septal perforation.
 Septal Perforation Vascular
Septal Perforation Vascular Septal Perforation No Vascular
Septal Perforation No Vascular Septal Perforation Dead Skin
Septal Perforation Dead Skin
Patients will sometimes ask, why can’t you just place a skin graft inside the nose? The reason for this is that the area where the perforation is has no blood supply. The skin graft will not “take” since the central portion does not receive blood. The reason for using a vascularized flap is that the flap has a blood supply to it, making it much more reliable. The benefit of this technique is that the flap is vascular. This creates blood flow into the perforation and allows for healing. If the flap was not vascularized, the skin would just die off.
FREQUENTLY ASKED QUESTIONS
Do all septal perforations need to be closed?
No, a septal perforation can be followed closely and seen if its size will change. Having observed many patients, Dr. Shah has seen patients who have had septal perforations, sometimes more than 25 years in age, which are small stay the same size over many years and patients have minimal symptoms. However, not all septal perforations are stable in size and some may require closure.
If my septal perforation is asymptomatic does it need to be closed?
A first step is to determine the size of the perforation and then see if it increases in size. If the perforation is not stable and the patient is symptomatic patients should consider closure of the perforation.
What is the most reliable technique for closing a septal perforation?
The best technique often involves tissue transfers with a stable blood supply. There is no one reliable technique for closing perforations and each approach has its pros and cons.
Why not just place a skin graft or graft from inside the mouth?
While more practical and technically easier to harvest and perform, these grafts typically do not survive. The reason is that the blood supply from a perforation is compromised. Placing free tissue over a perforation where there is limited blood supply will typically not allow enough vascular in growth to allow the graft to survive.
Why isn’t a free flap used more often?
A free flap can be used to close septal perforations somewhat reliably. The first issue is that there is a donor site typically from the forearm and more commonly the fascia along the leg. A free flap can involve multiple stages depending on the exact technique. It can be advantageous since it connects blood vessels to the flap making it reliable in closure of large perforations.
Can you guarantee a septal perforation closure?
No surgeon can guarantee closure of a septal perforation. The tissues of every patient and characteristics of each perforation are unique.
What technique do you use for larger septal perforations?
Larger septal perforations have an issue of not having enough tissue within the nose to close the perforation. In these cases, recruiting tissues from either the surrounding areas or via free flap can sometimes help to close a septal perforation. Asymptomatic large septal perforations which have been present for years may not have to be closed. Ironically, large septal perforations are often less symptomatic than smaller septal perforations.
If I have a septal perforation closure, when can I work out?
Working out for patients will start at the earliest at 4 weeks after closure. Patients should not work out until given clearance to do so.
When can I blow my nose?
Patients should wait for clearance to blow their nose. Violent nose blowing can cause a septal perforation in patients and should never be performed, even if the patient does not have a septal perforation.
Are some patients at risk for septal perforations?
Patients with poor mucosal hygiene (dry noses) and patients with previous septal surgery at higher risk for septal perforation with nasal interventions which includes nasal sprays, violent nose blowing and nasal surgery.
Are septal buttons a good option?
Septal buttons are used to provide a plastic spacer between the perforation. Septal buttons have been used for many years. The main issue is that the button often causes irritation to the surrounding tissues and is not tolerated well by most patients.
Do I need to have an incision on my scalp?
Yes, for a large perforation technique patients need to have an incision which can be difficult to see once it has healed. Access to the flap is otherwise difficult.
Do other surgeons perform this technique?
There are 2 case reports in the literature about this technique, one of which is described in 2002 and another more recently. Both surgeons utilize a coronal incision where a large incision is made along the scalp. To our office’s knowledge, no other surgeon uses an endoscopic technique to close perforations and other offices do not use this flap.
Is this procedure technically difficult?
Yes, moving a tissue paper thin graft from the forehead to the nose requires master knowledge on the following:
– Forehead anatomy and pericranial architecture including blood supply variation
– Nasal anatomy including function and grafting to the nose
Will I need rib cartilage?
Many patients will potentially need grafting due to the perforation collapsing the cartilage causing a saddle nose.
How large of a perforation has Dr. Shah closed with this technique?
Dr. Shah has closed near total perforations.
Is this technique guaranteed to close my perforation?
No technique in surgery is a guarantee. Using the sliding flap technique is limited to perforation sizes around 1.5 cm and sometimes up to 2 cm but often with success rates lower than 80% (reported in medical literature) to as low as 30% success rates. The forehead lining approach allows for perforations larger than 2 cm to be closed.
Will my nose feel different after repair with my forehead lining?
Our patients to date do not notice dryness after repair. The reason is theorized that the forehead lining serves as a scaffold for the surrounding mucosa to cover the nose. The main improvement is a feeling of comfort and improvement in the way the nose feels do to restoration in nasal air physiology.
Is this procedure painful?
While rhinoplasty and forehead lifts are typically not painful, there is some discomfort afterwards more than either procedure.
Is this procedure take a long time to heal?
Yes, the procedure takes about 6 weeks for the patient’s lining to heal. Patients are not advised to blow their nose or perform heavy activity during this time.


