
Prevention Of Lower Eyelid Malposition after Blepharoplasty
Abstract:
Objective: Determine the position of the lower eyelid and lateral canthus after release of the lower lid retractors with the “inside-out technique” by measuring the MR2 and use of the lateral canthal rounding scale.
Design: Retrospective analysis
Results: 78 of the 171 patients with the ‘inside out blepharoplasty’ had follow up of 3 months. Preoperative MR2 distance was found to be (.942). Postoperatively the modified MR2 distance was found to be (.903). The score of the modified MR2 distances were found to decrease postoperatively but this was not found to be statistically significant (p <.07 for observations on one>
No complications were reported.
Conclusion: The study found no difference in lateral canthal shape or MR2 distances between pre and postoperative photographic analysis patients who received the inside-out blepharoplasty.
The goals of lower eyelid rejuvenation are to restore youthful contours to the face while minimizing any complications or stigmata of surgery. A central tenet t of this goal is maintenance of lower eyelid position. The aesthetically pleasing lower eyelid is described as having a slight elevation laterally with little or no rounding. As part of the normal aging process, the lower lid may droop or round, leading to an unsightly cosmetic appearance. Aside from extraneous considerations, lower eyelid retraction can lead to serious functional morbidities such as ocular irritation, conjunctivitis, epiphora, blurred vision, and photophobia. (1)
Maintenance of lower eyelid position is crucial for the facial plastic surgeon to achieve satisfactory blepharoplasty results. Lower eyelid malposition may range from lateral canthal rounding to scleral show to frank ectropion. There are two basic surgical approaches to aesthetic rejuvenation of the lower lids: transcutaneous and transconjuctival. Subciliary blepharoplasty has been associated with lower eyelid retraction rates of up to 20%. (2-4) Transconjuctival blepharoplasty has a much lower rate of eyelid malposition, even with incorporation of transcutaenous skin removal or resurfacing. (5)
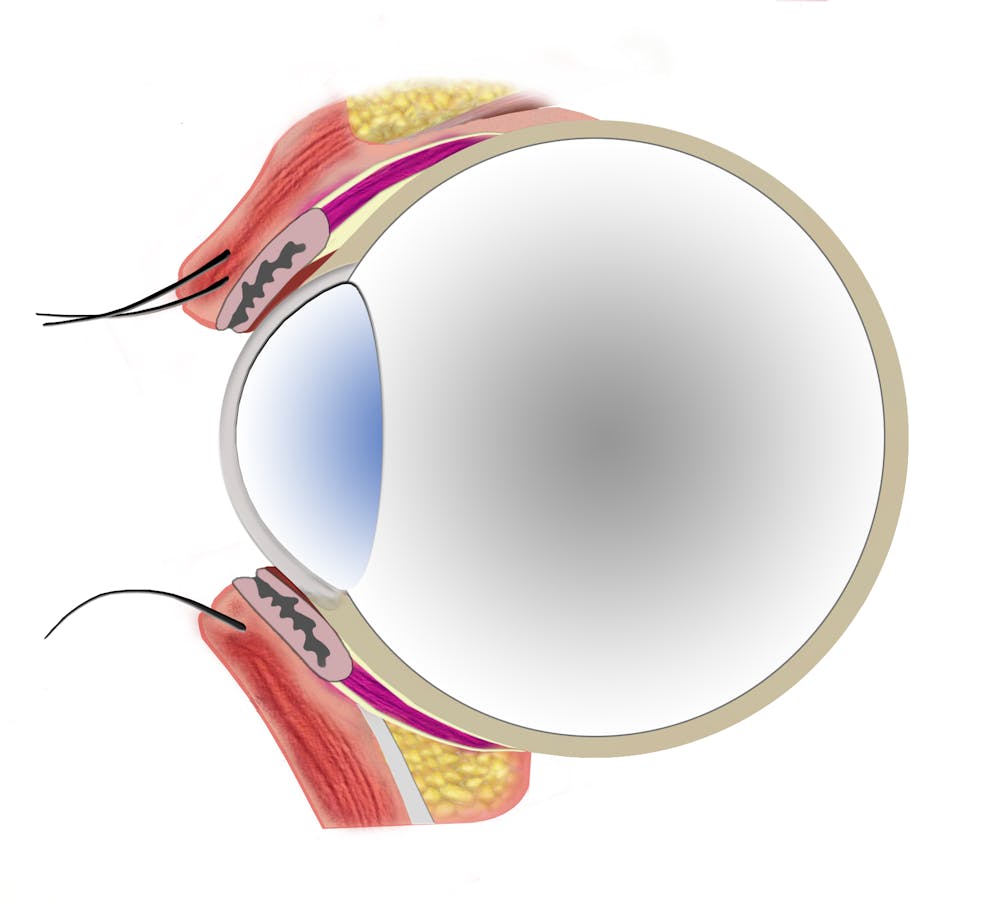
The factors responsible for lower eyelid position include canthal integrity, muscular dynamics and tonicity. (6) Typically, the lateral canthal tendon is slightly superior to the medial canthus, providing a natural pleasing slight elevation to the lateral portion of the lower eyelid. In patients with appropriate canthal strength, muscular dynamics play a role in the prevention of the lower eyelid malposition. Hypotonicity in the orbicularis oculi may lead to ectropion without resupport of the canthal tendon, as seen in patients with facial nerve paralysis. (7) The forces responsible include a weakened orbicularis oculi superior pull combined with the downward vector created by the inferior lid retractors and gravitational pull of soft tissues of the lid-cheek area.
Anatomic studies have led to further insight of the anatomy and function of the lower eyelid. (8-11) The retractors of the lower eyelid are analogous to those of the upper lid. The capsulopalpebral fascia (CPF) and the inferior tarsal muscle are directly comparable to the upper lid retractors of the levator aponeurosis and lower eyelids. The CPF originates from the fascia of the inferior rectus muscle and inferior oblique muscle and attaches to the inferior tarsus. The CPF pulls the lower tarsus downward, synchronized with the movement of the inferior rectus muscle. When the globe turns upward on eyelid closure (Bell’s phenomenon), the orbicularis oculi muscle contracts, and the inferior rectus and CPF relax. The orbicularis oculi and CPF are thought to be synchronized by reciprocal innervation in which there is an agonist/antagonist relationship.
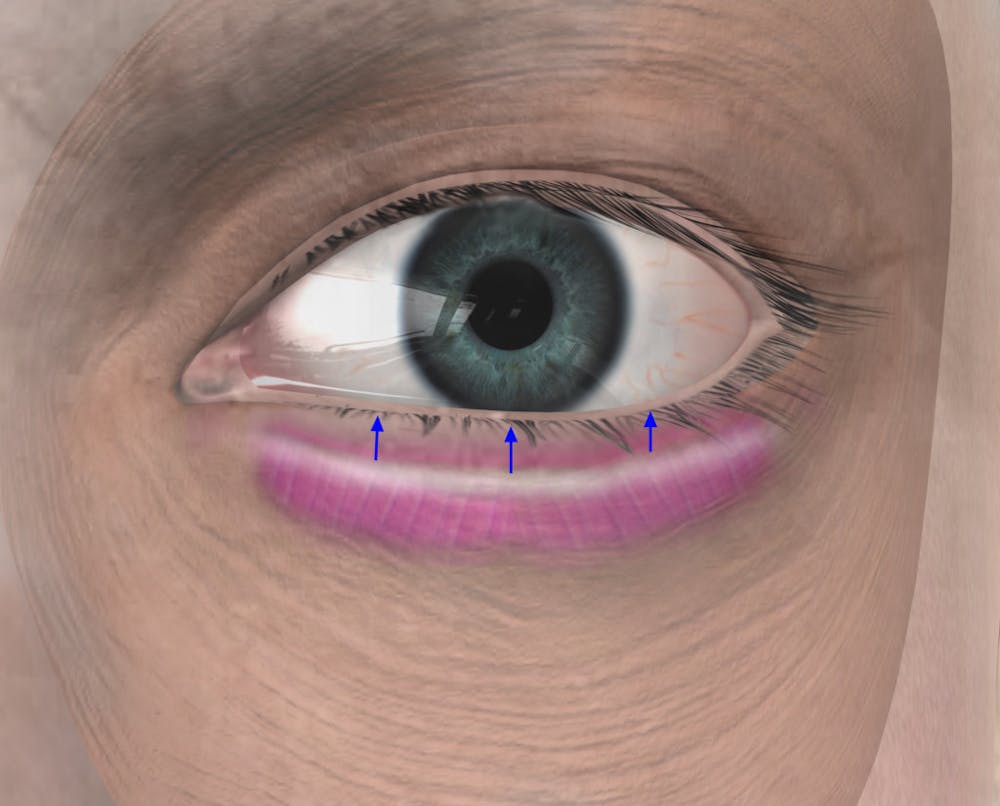
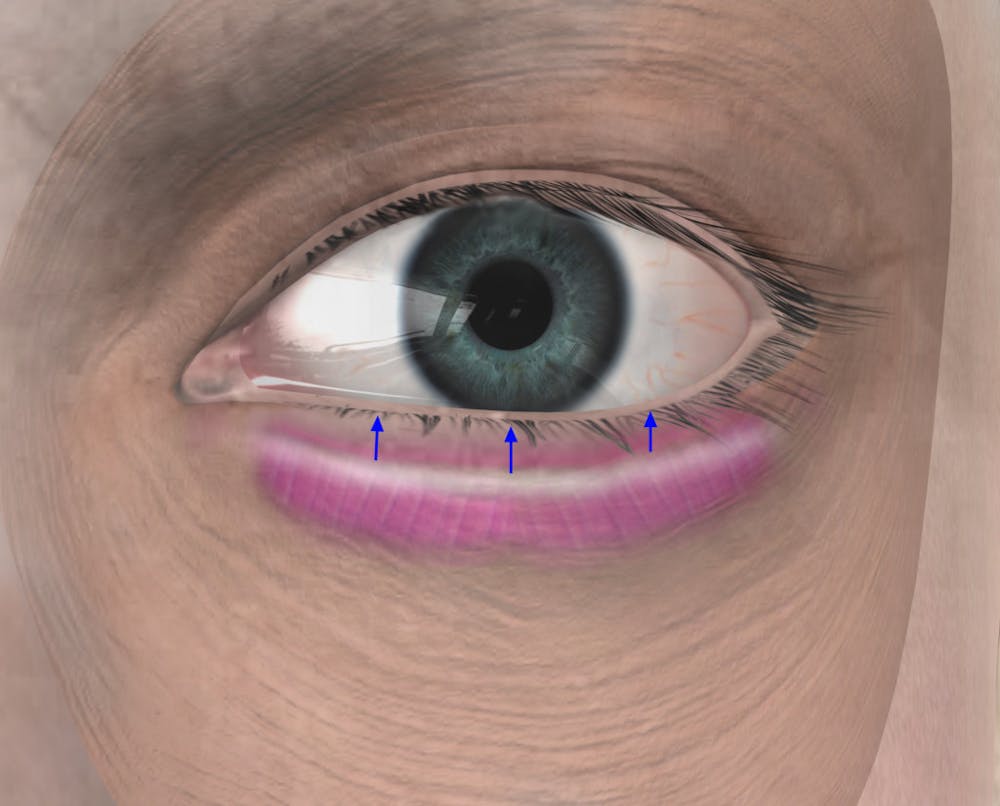
In upper eyelid surgery, if the levator aponeurosis, the upper eyelid retractor, is divided during upper blepharoplasty surgery, a postoperative ptosis will likely occur. During transconjuctival blepharoplasty, division of the lower eyelid retractors occurs. Preservation of the lateral tarsal orbicularis oculi’s innervation leads to an unopposed superiorly based muscular vector pull, manifesting as either maintenance or elevation of the lower eyelid. (Figure 1) The authors’ theorize that alteration of muscular dynamics plays an important role in preservation of lower eyelid position.
Materials and Methods:
A retrospective chart review was performed on the senior author’s patients from 2002-2005. 171 charts were identified as having had an inside-out transconjuctival blepharoplasty performed by the senior author. Exclusionary criteria included prior history of blepharoplasty or midface procedures and patients without postoperative pictures of at least 3 months follow up. Patients were excluded with prior blepharoplasty due to technical factors which could not be accounted for such as, preservation of orbicularis oculi supply, complete release of the lower eyelid retractors, or septal scarring.
All patients had preoperative assessment of canthal integrity (snap test, lid distraction distance), and were screened for dry eye. Patients with canthal laxity were addressed with lateral canthal shortening procedures and were excluded from this study.
Standardized blepharoplasty photographs were taken including a frontal view in neutral gaze, with eyes closed, and upward gaze and corresponding lateral views. Photographs were taken with a Sony Cyber Shot DSC-F828 camera (Tokyo, Japan) with macrolens at reproduction ratio of 1:4.
Postoperative photographs were taken preoperatively and 6 months after surgery. Photographs were examined at 6 months by comparison of modified MRD2 distances and any physical signs of lower eyelid malposition (rounding, increased scleral show, frank ectropion). Modified MRD2 was measured on all preoperative photographs as were any signs of lower eyelid malposition. Modified MRD2 is the measure of the light reflection in primary gaze to the lower eyelid lash line. The lash line was used rather than the lid margin to better account for lid eversion. (Figure 2) A standardizing multiplier was created to compare pre and postoperative photography by using the fixed point of the interpupilllary distance. Measures took place with the measure tool on Adobe Photoshop 7.0 (Santa Clara, CA).
A scale was created to measure lateral canthal rounding. (See Table 1) Authors were blinded to pre or post operative photographs and grading was performed for each eye. In addition, postoperative physical exam was performed to determine the mobility of the lower eyelid structures and formation of cicatrix. Statistics were analyzed with one-tailed Student’s t-test and significant values were considered less than p<.05.>
Technique- The Inside-out Blepharoplasty
Patients were marked in the preoperative holding area where significant fat herniation was identified. All procedures were performed under general anesthesia. Corneal shields with bacitracin ophthalmic were placed during the surgery. A local anesthetic mixture (1% lidocaine with 1:100,000 epinephrine on a 30 gauge needle) was injected into the lower eyelid conjunctiva in all patients and transcuteanously location if skin removal was planned.
(The In)
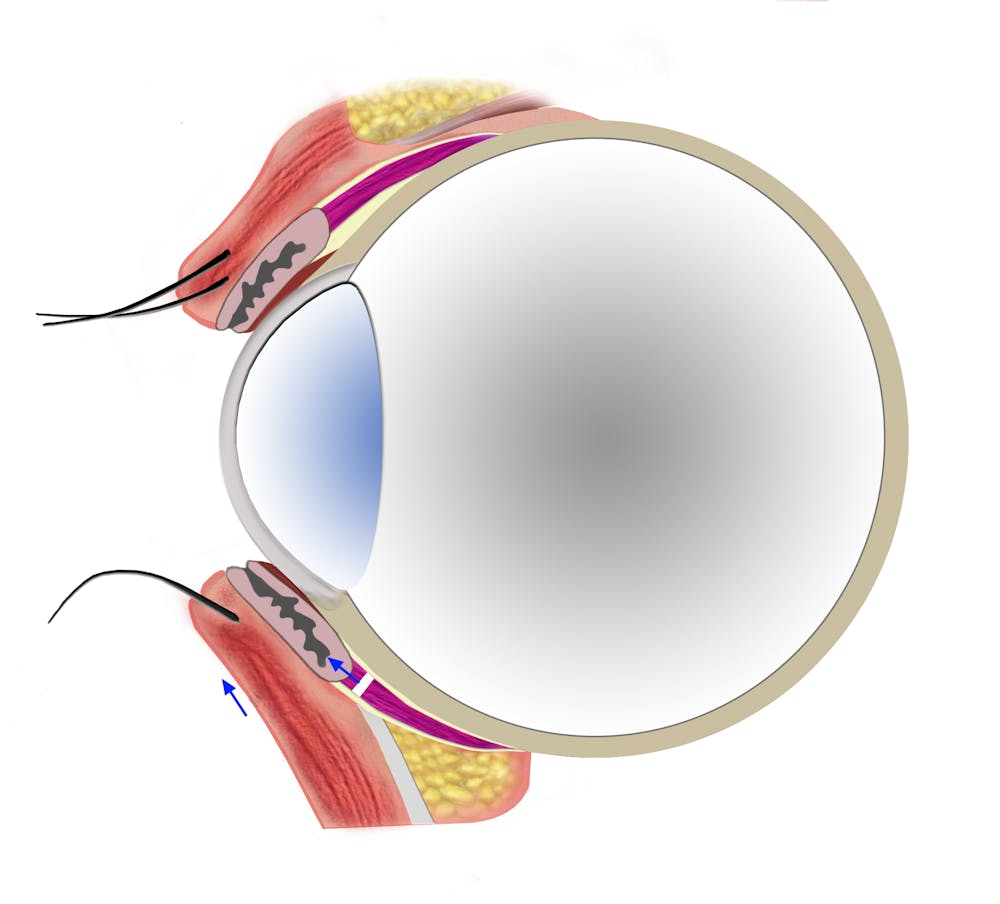
Transconjuctival approach was utilized to facilitate access to the fat compartments and release the lower lid retractors. The lower eyelids were retracted with a sharp double pronged retractor. An incision was made with a guarded Colorado tip needle 1 mm from the tarsal border along the lower lid conjunctiva. The incision was extended from the medial puncta to the just medial to the lateral canthus to ensure complete release of the lower eyelid retractors, irrespective of the location of fat removal. A preseptal plane was dissected bluntly in an avascular plane with a cotton-tipped applicator to the level of the orbital rim.
Fat was removed only in those areas where preoperative analysis revealed excess.
The fat was removed to allow a 1 mm smooth level of fat below the orbital rim. The inferior oblique muscle was identified in all cases where fat was removed. Fat repositioning was not performed and nasojugal asymmetries were addressed with fat transplantation techniques. The transconjuctival incision was not closed to allow for egress of fluid and to prevent reapproximation of the lower lid retractors. (Figure 3)
(The Out)
Transcutaneous removal of skin was utilized in all cases. An incision with a 15 blade was made at the lateral border of the lower eyelid, following a lower eyelid crease. Straight stevens scissors were used to dissect 3 mm from the border of the lower lid margin to the medial puncta. The transcutaneous flap was elevated and skin was removed so that no tension was placed on the closure of the skin. 6-0 prolene suture was used in a running nonlocking fashion. In instances of excessive muscular orbicularis oculi, a small portion of the septal oribicularis oculi was resected, preserving the tarsal orbicularis oculi. .
Postoperative care consisted of aggressive lower lid massage for 2-4 weeks to prevent cicatrix formation.
Results:
78 of the 171 patients with the inside out blepharoplasty had follow up of 3 months. Preoperative MR2 distance was found to be (.942). Postoperatively the modified MR2 distance was found to be (.903). (See Figure 4)
The score of the modified MR2 distances were found to decrease postoperatively but this was not statistically significant (p<.07 months>
The lateral rounding scale reviewed an average score of (2.04) for preoperative patients and (1.99) for postoperative patients. There was not a statistical difference between pre and postoperative observations based on a one tailed t-test.
No complications were reported including hematoma and postoperative dry eyes. Patients did not demonstrate entropion or decreased ability to look downward as a result of the lower lid retractors on physical exam.
Discussion:
Several technical factors bear mentioning in the inside-out technique. The release of the retractors is complete and occurs from medial puncta and approaches the lateral canthus of the eye. Retractor release does not typically occur with a subciliary approach with preservation of the underlying conjuctiva and associated lid retractors. Both a pre or postseptal approach will theoretically provide release of the retractors.
A function of the lower lid retractors is to assist in lowering the eyelid, particularly when the inferior rectus muscle pulls the eye inferiorly. Despite this contribution to lid lowering, no reports of inferior gaze restriction or discomfort have been reported after transconjuctival blepharoplasty. Our study supports the literature with none of the patients reporting gaze restriction after release of the lower lid retractors.
Putterman described a sole case of ectropion as a result of resection of the lower eyelid retractors. (12) However, this case example had severe lateral canthal laxity, and no subsequent cases of ectropion have been reported.
Epiblepharon was reported in a subciliary approach for a case in an Asian patient after repair of a trimalar fracture. (13) In Asian patients, the capsulopalprepal fascia is attenuated with weaker attachement to the tarsal plate and dermis. There is a much higher incidence of epiblepharon in Asian patients due to the unopposed muscular force vector provided by the orbicularis oculi muscle. Epiblepharon has never been reported after a transconjuctival blepharoplasty. The downward effects of gravity and shortening of the middle lamellae during surgery are possible explanations for the lack of this phenomenon in postblepharoplasty patients.
DiFrancesco performed an EMG study on the orbicularis oculi after subciliary blepharoplasty and found maintenance of tone and innervation after subciliary blepharoplasty. (14) The main difference between a standard subciliary approach blepharoplasty and the inside-out approach is the resection of the lower lid retractors. While subciliary blepharoplasty patients have much higher rates of lower lid malposition, the inside-out blepharoplasty and standardized transconjuctival blepharoplasty patients do not seem to suffer from lid malposition. Clearly, the transection of the lower lid retractors plays a role in the preservation of eyelid position in these patients.
Lateral rounding and lid positioning remained unchanged after surgery despite transcutaneous skin removal and TCA peels. The inside-out blepharoplasty offers a safe alternative to standard subciliary blepharoplasty in achieving commendable aesthetic results without compromising lid position or canthal integrity.
Conclusion:
Maintenance of lower lid position after lower lid blepharoplasty is a difficult endeavor. Few studies have critically examined with objective measures the MR2 distances. A lateral canthal rounding scale was developed to provide additional analysis of the lateral canthal shape or MR2 distances between pre and postoperative photographic analysis patients who received the inside-out blepharoplasty.
References
1. Westfall CT, Shore JW, Nunery WR, Hawes MJ, Yaremchuk MJ. Operative complications of the transconjunctival inferior fornix approach. Ophthalmology. 1991 Oct;98(10):1525-8.
2. Patel PC, Sobota BT, Patel NM, Greene JS, Millman B. Comparison of transconjunctival versus subciliary approaches for orbital fractures: a review of 60 cases. J Craniomaxillofac Trauma. 1998 Spring;4(1):17-21.
3. Appling WD, Patrinely JR, Salzer TA. Transconjunctival approach vs subciliary skin-muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg. 1993 Sep;119(9):1000-7.
4. Holtmann B, Wray RC, Little AG. A randomized comparison of four incisions for orbital fractures. Plast Reconstr Surg. 1981 Jun;67(6):731-7.
5. Mullins JB, Holds JB, Branham GH, Thomas JR. Complications of the transconjunctival approach. A review of 400 cases. Arch Otolaryngol Head Neck Surg. 1997 Apr;123(4):385-8
6. Kakizaki H, Zako M, Nakano T, Asamoto K, Miyagawa T, Iwaki M.Three ligaments reinforce the lower eyelid. Okajimas Folia Anat Jpn. 2004 Dec;81(5):97-100.
7. Fedok FG, Ferraro RE. Restoration of lower eyelid support in facial paralysis.
Facial Plast Surg. 2000;16(4):337-43.
8. Goldberg RA, Lufkin R, Farahani K, Wu JC, Jesmanowicz A, Hyde JS. Physiology of the lower eyelid retractors: tight linkage of the anterior capsulopalpebral fascia demonstrated using dynamic ultrafine surface coil MRI. Ophthal Plast Reconstr Surg. 1994 Jun;10(2):87-91.
9. Hawes MJ, Dortzbach RK. The microscopic anatomy of the lower eyelid retractors. Arch Ophthalmol. 1982 Aug;100(8):1313-8.
10. Lim WK, Rajendran K, Choo CT. Microscopic anatomy of the lower eyelid in asians.Ophthal Plast Reconstr Surg. 2004 May;20(3):207-11.
11. Wojtowicz S. Reciprocal innervation of directly and indirectly synergic and antagonistic external eye muscles. Pol Med J. 1966;5(3):656-61.
12. Putterman AM. Ectropion of the lower eyelid secondary to Muller’s muscle-capsulopalpebral fascia detachment. Am J Ophthalmol. 1978 Jun;85(6):814-7.
13. Park RI, Meyer DR. Acquired lower eyelid epiblepharon. Am J Ophthalmol. 1996 Sep;122(3):449-51.
14. DiFrancesco LM, Anjema CM, Codner MA, McCord CD, English J.Evaluation of conventional subciliary incision used in blepharoplasty: preoperative and postoperative videography and electromyography findings. Plast Reconstr Surg. 2005 Aug;116(2):632-9.
Table 1. Eye Rounding Scale
1 = no lateral canthal rounding or eversion, (canthal angle acute)
2 = minimal lateral canthal rounding, (canthal angle moderately enlarged with minimal rounding)
3 – moderate lateral canthal rounding with some lid eversion (moderate canthal angle distance with rounding)
4 – severe lateral canthal rounding (marked canthal rounding and obtuse canthal angle)
Figure 1a. Normally, the orbicularis oculi exerts a slight superior force on the lower lid, while the lower lid retractors exert a slight inferior force mitigating a directional pull on the lower lid.
Figure 1b. After resection of the lower lid retractors, the orbicularis oculi exerts an unopposed superior force on the lower lid.
Figure 2a. The lower lid retractor can be approached through a transconjuctival incision.
Figure 2b. With release of the transconjuctival approach, the orbicularis oculi will exert a slight superior force on the lower lid.
Figure 3. Immediately after resection of the lower lid retractors, it is evident that the lower lid on the right is now superior than the lower lid on the left.
Figure 4. Patient demonstrates maintenance of lower lid position and the aperture of the eye has not changed due to the lateral canthal angle not changing significantly.
Figure 5. Patient demonstrates unchanged position of lower lid and aperture of the eye in pre and postoperative photographs.
Figure 6. Patient with slight improvement of the position of the lower eyelid with minimal change to lateral canthal angle.


