Nasal septal deviation in the pediatric and adult populations
Abstract
A significant proportion of the population has nasal septal deviation of varying degrees. Recent reports of such deviation occurring at younger ages suggest a congenital etiology. To the best of our knowledge, no previous clinical studies have compared the septal deviation of adult and pediatric populations with a uniform measure that focuses on the degree of deviation. We retrospectively analyzed computed tomography (CT) and magnetic resonance imaging (MRI) scans obtained from 81 patients who had undergone head and neck imaging for a variety of reasons. These subjects were divided into four age groups: younger than 4 months; 4 months to less than 5 years; 5 to 15 years; and more than 15 years. We used a measure of tortuosity to examine and compare nasal septal deviation among the different age groups. The tortuosity of the septum was measured at four precise points along the length of the septum on thin-section sinus CT and MRI. Tortuosity was defined as the ratio of the “actual” length of the septum to the “ideal” length of the septum, which was defined as the length of a straight line drawn from the superior to the inferior aspect of the septum. We found that subjects younger than 5 years of age exhibited significantly less tortuosity (p ≤ 0.017459) than did the older children and the adults. Therefore, we conclude that nasal septal deviation occurs at a higher frequency in older children and in adults when calculations of tortuosity are used as a measure. Our data may suggest that a noncongenital etiology is responsible for nasal septal deviation. However, given that the growth of the septum continues throughout childhood, our results do not preclude the possibility of a genetic predisposition to the later development of a deviated nasal septum.
by Shari D. Reitzen, MD, Wayne Chung, MD, and Anil R. Shah, MD
Introduction
Numerous studies of nasal septal deviation have revealed a wide range of prevalence.1-6 In 1978, Gray reported a prevalence of 48 to 60% in neonates.1 In subsequent reports, prevalence in newborns ranged from 0.93%2 to 22%.3 In older children, studies have shown a prevalence of 12.4% in children aged 2.5 to 6 years old4 and 13.6% in 6- to 9-year-olds.1,5 In adults, a recent international study found a prevalence of approximately 90%.6 Considering the wide variety of findings, the true prevalence of nasal septal deviation is unknown.
The widely varying nature of these findings can be explained in part by the fact that different age groups have been studied and that several classification systems have been used. Moreover, in many of these classification systems, deviation is evaluated at only one specific point along the entire septum. However, since septal deviation can occur at any point from the naris to the choana, a classification system based on only one part of the septum tends to underestimate the prevalence of deviation.
Although studies that have included both pediatric and adult populations have been reported, to the best of our knowledge no direct comparison of these populations based on a uniform measure of the degree of deviation has been previously reported. In this article, we describe our study, in which we used a standardized measure of tortuosity to compare the amounts of deviation among several different age groups.
Patients and methods
We obtained thin-section sinus computed tomography (CT) and magnetic resonance imaging (MRI) scans from 81 adult and pediatric patients who had been seen at our tertiary care referral center for all causes from Jan. 1 through Dec. 31, 2006. The ages of the patients ranged from 2 months to 80 years. The study population was divided into four age groups: younger than 4 months (n = 3); 4 months to less than 5 years (n = 31); 5 to 15 years (n = 27); and more than 15 years (n = 20).
The CT scans had been performed in a GE HiSpeed CT/I scanner (GE; New York City). The scanner yielded 2.5- to 3.0-mm axial, coronal, and sagittal studies of the septum and paranasal sinuses. MRI had been performed in a Siemens 3T scanner (Siemens AG; Malvern, Pa.). Scans that contained motion artifact and those that had been obtained from patients with a history of trauma were excluded; otherwise, patients’ histories were not taken into account.
The CT and MRI images were imported into a Vitrea workstation (Vital Images; Minnetonka, Minn.). The images were measured with the ruler function. In the axial and sagittal views, images were centered on the midline. A point from anterior to posterior was chosen on the sagittal scan to serve as a reference point for the coronal measurements. The length of the septum was measured in the coronal plane from the cribriform plate superiorly to the hard palate inferiorly. Tortuosity was calculated by dividing the “actual” length of the septum by the “ideal” length, which was the length of a straight line from the starting point (superior aspect of the septum) to the ending point (inferior aspect of the septum). Septal deviation was measured at four different points along the cartilaginous and bony septum. The actual length and the ideal length were each measured at the piriform aperture, at the choanae, at half the distance from the tip of the nose to the piriform aperture, and at half the distance from the piriform aperture to the choanae (figure). The point of maximum tortuosity was used in defining the degree of septal deviation in each patient.
Measurements were compared with the paired-samples Student t test and were expressed as mean values. A p value of less than 0.05 was accepted as statistically significant.
Results
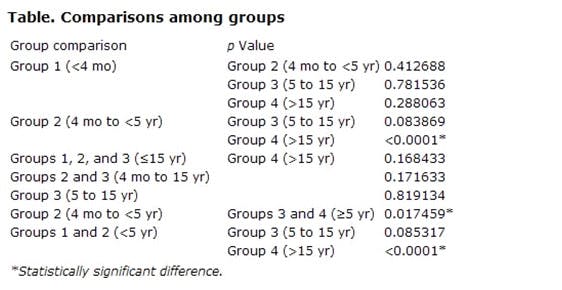
A total of 11 comparisons were made among various age groups. Statistically significant differences were seen in three of these comparisons, all of which indicated that nasal septal deviation occurs at a higher frequency in older children and in adults when calculations of tortuosity are used as a measure (table).
Discussion
Nasal septal deviation has been classified and quantified in several ways. Mladina et al classified septal deformities on the basis of their vertical and/or horizontal orientation.6 Cottle et al classified them into four types: subluxation, large spur, caudal deflection, and tension septum.7 Guyuron et al used a six-category system: septal tilt, anteroposterior C-shape, cephalocaudal C-shape, anteroposterior S-shape, cephalocaudal S-shape, and wide spurs.8 Buyukertan et al classified them by separating the nasal septum into 10 segments to better localize the deformity.9
Obviously, establishing a consensus on one standardized classification system would be helpful in many ways. We used an absolute measure to produce a value that represents a degree of deviation. What distinguishes our method from the others is that it takes into account the natural curve of the septum. Our quantification of tortuosity provides an indication of how much the septum deviates from the midline at each particular point measured. (It is important to note that our method cannot be used to draw conclusions regarding the airflow of the nose because it does not account for other nasal structures [e.g., the turbinates] or pathology [e.g., mucosal edema].)
In our study, the younger children generally had lower rates of tortuosity than did the older children and the adults (table). We cannot draw any conclusions about the neonates (group 1) because only 3 subjects younger than 4 months were included in this study. In addition, none of the children with nasal septal deviation had been followed from birth, so we cannot determine if they had a nasal septal deviation at birth or if they acquired it later on. Possible explanations for the later acquisition of a nasal septal deviation include trauma and a genetic predisposition in which a nasal septal deviation forms during the growth and development of the facial skeleton. Studies have shown that the prevalence of certain types of nasal septal deviation (i.e., posterior deflections) increases with age while the prevalence of others (i.e., anterior deflections) decreases with age; these findings are believed to have occurred as an effect of the growth of the nasomaxillary complex.10,11
Our data seem to suggest that there is not a congenital component to the etiology of nasal septal deviation. Indeed, it has been suggested by many authors that septal deformities in newborns are largely attributable to birth injury. As newborns are obligate nose breathers, nasal septal deviation can cause respiratory compromise. According to Kawalski and Spiewak, neonates born with nasal septal deviation encounter respiratory issues when coincident mucosal edema leads to a total blockage of the nasal cavity.3 This total nasal obstruction leads to choking and aspiration when feeding, and it has been reported as a possible cause of sudden infant death syndrome. Therefore, close observation of neonates with nasal deviation is recommended.

Figure. Tortuosity is measured at four precise points along the length of the nasal septum. Tortuosity is quantified as the ratio of the actual length of the septum (T) to the ideal length (I)-that is, T/I = Ratio. In this particular case, T had a value of 32 and I had a value of 31.1, yielding a ratio of 1.03. In the four images along the bottom, the purple lines represent the actual length (T) and the blue lines represent the ideal length (I).
The study by Kawalski and Spiewak involved 273 newborns; anterior septal deviation was found in 49 of 221 (22%) of those who were delivered spontaneously and in 2 of 52 (3.8%) of those who were delivered via cesarean section.3 The frequency of posterior nasal septal deviation was the same in the two groups. Kawalski and Spiewak also reported that the anterior septum straightened spontaneously during the first 3 days of life.
Podoshin et al analyzed the cases of 4,090 neonates who had been born without any evidence that birth trauma had been the cause of congenital nasal deformity.2 They proposed that most of these dislocations had occurred during intrauterine life. Therefore, they suggested that the role of birth injury as an etiologic factor in nasal septal deformities in newborns is unclear.
Sooknundun et al reported a septal deviation prevalence of 15 to 25%.12 They concluded that uncorrected deviation results in more frequent infections and other problems, such as mouth breathing and feeding difficulty. They advocated early intervention (closed reduction) at birth. After 5 years of follow-up, their patients were noted to have had a stable reduction. Thus, they concluded that the etiology of nasal septal deviation among children might indeed have a congenital component.
There are several limitations to this study. First, our measurements were obtained from two different radiologic modalities (CT and MRI). Second, the CTs and MRIs were obtained from subjects who were likely to have had some head and neck pathology. Third, these images were obtained from among a random group of radiologic scans, regardless of the possible nature of the subject’s health status. Finally, our study population did not include an adequate number of neonates (n = 3).
In conclusion, our findings suggest that nasal septal deviation is more common in older children and adults when its presence is defined on the basis of calculations of tortuosity. Our data may support a noncongenital etiology for nasal septal deviation. However, given that the growth of the septum continues throughout childhood, our results do not preclude the possibility of a genetic predisposition to the later development of a deviated nasal septum.
From the Division of Facial Plastic & Reconstructive Surgery, Department of Otolaryngology, New York University School of Medicine, New York City (Dr. Reitzen, Dr. Chung, and Dr. Shah); and the Division of Facial Plastic & Reconstructive Surgery, Department of Otolaryngology-Head and Neck Surgery, Manhattan, Eye, Ear & Throat Hospital, New York (Dr. Shah).
Previous presentation: The information in this article has been updated from its original presentation as a poster at the Combined Otolaryngology Spring Meetings; May 1-4, 2008; Orlando, Fla.
Corresponding author: Shari D. Reitzen, MD, Department of Otolaryngology, New York University School of Medicine, 550 First Ave., NBV 5E5, New York, NY 10016. E-mail: [email protected]
References
Gray LP. Deviated nasal septum. Incidence and etiology. Ann Otol Rhinol Laryngol Suppl 1978; 87 (3 Part 3 Suppl 50): 3-20.
Podoshin L, Gertner R, Fradis M, Berger A. Incidence and treatment of deviation of nasal septum in newborns. Ear Nose Throat J 1991; 70 (8): 485-7.
Kawalski H, Spiewak P. How septum deformations in newborns occur. Int J Pediatr Otorhinolaryngol 1998; 44 (1): 23-30.
Van Cauwenberge P, Derycke A. The relationship between nasal and middle ear pathology. Acta Otorhinolaryngol Belg 1983; 37 (6): 830-41.
Song SY, Kim IT, Chang KH, et al. The prevalence of nasal septal deformities among children in kindergarten and first grade in Anyang and Kunpo cities. J Rhinol 1999; 6 (1): 58-60.
Mladina R, Cujić E, Subarić M, Vuković K. Nasal septal deformities in ear, nose, and throat patients: An international study. Am J Otolaryngol 2008; 29 (2): 75-82.
Cottle MH, Loring RM, Fischer GG, Gaynon IE. The maxilla-premaxilla approach to extensive nasal septum surgery. AMA Arch Otolaryngol 1958; 68 (3): 301-13.
Guyuron B, Uzzo CD, Scull H. A practical classification of septonasal deviation and an effective guide to septal surgery. Plast Reconstr Surg 1999; 104 (7): 2202-9; discussion 2210-12.
Buyukertan M, Keklikoglu N, Kokten G. A morphometric consideration of nasal septal deviations by people with paranasal complaints; a computed tomography study. Rhinology 2003; 41 (1): 21-4.
Subarić M, Mladina R. Nasal septum deformities in children and adolescents: A cross sectional study of children from Zagreb, Croatia. Int J Pediatr Otorhinolaryngol 2002; 63 (1): 41-8.
Zielnik-Jurkiewicz B, Olszewska-Sosińska O. The nasal septum deformities in children and adolescents from Warsaw, Poland. Int J Pediatr Otorhinolaryngol 2006; 70 (4): 731-6.
Sooknundun M, Kacker SK, Bhatia R, Deka RC. Nasal septal deviation: Effective intervention and long term follow-up. Int J Pediatr Otorhinolaryngol 1986; 12 (1): 65-72.
Ear Nose Throat J. 2011 March;90(3):112-115