
Nasal Reconstruction of the Leprosy Nose Using Costal Cartilage
Anil R. Shah MD, Daniel Zeitler MD, and Jeffrey B. Wise MD*
Anil R. Shah MD
Clinical Instructor, Division of Facial Plastic Surgery, Section of Otolaryngology, University of Chicago
Chicago, IL
Private Practice, Chicago, IL
Daniel Zeitler MD
Resident, Department of Otolaryngology, New York University School of Medicine, New York, NY
Jeffrey B. Wise MD
Clinical Assistant Professor, Division of Facial Plastic Surgery, Department of Otolaryngology, New York University School of Medicine, New York, NY
Private Practice, Wayne, NJ
Corresponding Author for Proof and Reprints:
Jeffrey B. Wise, MD
1680 Route 23, Suite 100
Wayne, NJ 07470
[email protected]
973.305.1400
973.684.5580 (fax)
Coauthors addresses:
Daniel Zeitler MD
Department of Otolaryngology
New York University School of Medicine
462 First Avenue and 27th Street, NBV 5E 5
New York, NY 10016
212.263.6344
Anil R. Shah MD
200 West Superior St., Suite 200
Chicago, IL 60654
312.944-0117
KEYWORDS
Saddle-nose deformity
Leprosy
Autogenous costal cartilage graft
ABSTRACT
Leprosy is a chronic granulomatous infection of the skin and peripheral nerves that often leads to gross deformation of the nasal skeleton and subsequent formation of a saddle-nose deformity. Reconstruction of the nose following Mycobacterium leprae infection has challenged surgeons for centuries. As a result, a number of different techniques have been attempted with varying outcomes. We describe the case and surgical treatment of a 37-year old female who presented with a subtotal nasoseptal perforation and saddle-nose deformity secondary to previous infection with leprosy. Reconstruction was achieved via an open septorhinoplasty approach using autologous costal cartilage grafts, yielding a successful postoperative result.
Leprosy is a chronic granulomatous infection of the soft tissue of the skin and peripheral nerves that has plagued industrialized human populations worldwide for thousands of years. Leprosy remains a commonly occurring disease in some countries, with over 219,000 cases reported and a prevalence of more than one case per 10,000 people [1]. Unfortunately, despite medications that can effectively treat leprosy, it remains a difficult disease to detect, and diagnosis often occurs after the onset of several specific deformities. One of the most common manifestations of leprosy is the destruction of nasal cartilage – interestingly, this disease universally preserves the skin, mucosa, and lower lateral cartilages of the nose.
Believed to have originated in the Indian subcontinent, the disease traversed the globe from Europe to Africa, along with the Far East and South America. However, since the description of the causative etiologic agent, Mycobacterium leprae, in 1873 by Gerhard HA Hansen, the disease has become concentrated mostly in resource-poor countries within tropical climate zones. Currently, 83% of recorded cases of the disease are found in only six countries: India, Brazil, Burma, Indonesia, Madagascar, and Nepal [2]. Due to the large immigrant influx into major metropolitan cities within the United States, coupled with Leprosy patients frequently presenting with signs and symptoms of the disease long after leaving an endemic region, it is important that U.S. clinicians be able to diagnose and treat manifestations of this disease.
Although there are numerous functional and cosmetic consequences secondary to lepromatous disease, perhaps none is more distressing or socially stigmatized than the development of a saddle-nose deformity. Inhalation of the mycobacterium allows for infiltration of the nasal mucosa and subsequent destruction of the bony and cartilaginous skeleton along with the mucosal lining [3]. This results in extensive remodeling of the nasal framework and significant ensuing deformities. As such, surgeons have proposed a variety of reconstructive techniques, some of which include nasolabial turnover flaps [4], post-nasal skin grafts [5], silicone rubber implants and other external prostheses [5], and most recently, autologous auricular and/or costal cartilage grafts [6]. We present a case of severe saddle-nose deformity secondary to prior infection with Mycobacterium leprae (Leprosy), and successful reconstruction with autologous costal cartilage grafts.
Case Report
A 37-year old female born in the Dominican Republic, and a recent immigrant to the United States, presented with a complaint of complete nasal collapse. Her pertinent history began 7 years previously at age 30, when she sought medical attention from a dermatologist for multiple skin lesions developing on her upper extremities and trunk. A diagnosis of leprosy was made based on histological evidence, and the patient was treated for several months with “multiple antibiotics”. Beginning in her mid-30s, the patient began to note progressive changes in the structure of her nose, along with significant nasal obstruction. Gradually, she noticed her entire nose “collapse.” Family members and friends had difficulty recognizing her. The patient does not report a history of other family members contracting or having been treated for leprosy in the past. The leprosy has been “quiescent” for a period of 2 years since her last treatments, the details of which she did not recall.
Physical exam demonstrated a woman with a severe saddle nose deformity and total nasal septal perforation. The patient had decreased tip support and recoil, which resulted in a bulbous, underprojected nasal tip. Aside from significant middle vault collapse, she also demonstrated deficient premaxillary projection.


Figure 1A Figure 1B


Figure 1C Figure 1D

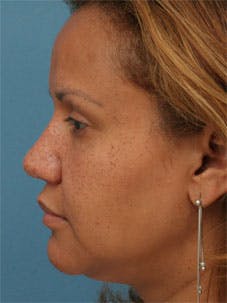
Figure 1E Figure 1F


Figure 1G Figure 1H
A nasal reconstruction was performed via an open rhinoplasty approach. Costal cartilage from two ribs, specifically the left seventh and eighth ribs, were harvested in order to repair her nose. Support of the nasal base was achieved with an extended columellar strut, carved from costal cartilage. The strut was carved to help project the nasal tip and augment the columella and premaxilla. The strut was not integrated with the residual septum.


Figure 2A Figure 2B
Two interrupted permanent sutures were placed through the periosteum along the nasal spine to stabilize the graft.

Figure 3A Figure 3B
In an effort to augment the premaxilla, several small pieces of costal cartilage (2 mm x 2 mm x 2 mm) were placed in a precisely made intranasal pocket and closed with 4-0 chromic gut sutures (Ethicon, Somerville, NJ).
A mild boney dorsal reduction was undertaken with a rasping technique to allow for a smooth platform for nasal dorsum augmentation. A thinly-sculpted dorsal onlay graft was placed over the nasal bones and upper lateral cartilages. The graft was carved from the soft central core of costal cartilage in an effort to mitigate the risk of cartilaginous warping. Furthermore, a moderately-crushed cartilagenous graft was placed over the middle third. Finally, the radix was augmented with remaining costal perichondrium.

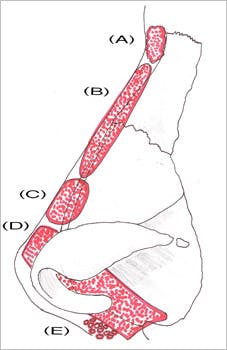
Figure 4
Leprosy Epidemiology
The pathology of nasal skeleton collapse in leprosy begins with nasal septal mucosal edema and subsequent destruction following infiltration with Mycobacterium leprae, an inhaled pathogen. The majority of patients with nasal collapse have long-standing disease [3]. Initially, the damage is microscopic; however, as the disease progresses, the destruction becomes visible on gross examination [7]. Once the nasal septal mucosa is destroyed, the underlying quadrangular cartilage is exposed leading to secondary bacterial infection. Alternatively, exposure necrosis may result secondary to vascular ischemia, with the loss of the perichondrial blood supply. The end result is septal perforation. Those structures covered by respiratory mucosa on both surfaces, including the nasal septum, nasal spine of the maxilla, and the turbinates, are most prone to destruction. As the nasal spine is resorbed, the classic saddle-nose deformity can develop, accompanied by an acute nasolabial angle and a deficiency of columellar show. Progression of the disease often occurs with partial or complete destruction of the nasal bones with resultant flattening of the nasal bridge. In rare cases, scar tissue retraction can lead to virtual elimination of the nasal vestibule, thereby causing significant functional deficits. Fortunately, it is exceedingly rare for the nasal skin-soft tissue envelope to be affected by the disease.
Leprosy Drug Regimen
Given the significant functional and aesthetic consequences of the lepromatous saddle-nose deformity, patients affected with the disease are often eager to undergo surgical correction. However, it is important that maximal medical management has been employed prior to operative intervention. In the 1990s, the recommendation for treatment of leprosy by the World Health Organization (WHO) involved 2 years of multidrug therapy (MDT) with rifampicin, dapsone, and clofazimine [8]. More recently, the recommended treatment duration was decreased to 12 months [9], with the newest recommendations for MDT courses as short as 6 months[10]. As there is little expert consensus and a dearth of long-term, controlled trials on the length of therapy, our recommendation is to ensure the patient has received an adequate medication trial while demonstrating no evidence of active lesions or continued mucosal/cartilaginous destruction prior to initiating operative planning.
Leprosy Saddle Nose Deformity Correction
Many authors have devised different classification systems for grading saddle-nose deformities in order to predict operative intervention and/or framework material needed for repair [3,6, 11-13]. However, in the published literature for repair of the leprosy saddle-nose to date, there is a tendency to use only one technique for all repairs based on the surgeon’s expertise or preference, or to use various techniques without a description of the indication for each type of repair [5, 14, 15]. Additionally, there is no consensus on the ideal implant material (i.e. autologous costal cartilage, homologous irradiated rib cartilage, auricular cartilage, allografts, or bone) for use in reconstruction of the saddle-nose, as each surgeon tends to hold individual preferences.
Augmentation for Severe Saddle Nose
While septal cartilage is seen by many as the ideal grafting material [16-19], its use is precluded in rebuilding the severe saddle-nose, as there is almost always a deficiency of viable cartilage. Thus, additional sources of grafting material must be utilized. Irradiated homologous rib cartilage (IHRC) is a practical option with principal advantages being avoidance of donor site morbidity and associated perioperative risks such as pneumothorax. Furthermore, IHRC is associated with low rates of infection and extrusion. However, reports on the resorption rates of IHRC used in rhinoplasty have been inconsistent, with many long-term results showing low or negligible graft resorption rates [20] while other series demonstrate resorption rates to be much higher [21, 22]. In the only published study on IHRC use in rhinoplasty for destructive diseases of the nasal framework, there was significant resorption of the irradiated rib cartilage that required multiple revision surgeries. The authors therefore recommend against using IHRC in such cases whenever possible [23].
Recently, Menger and associates [6] described their experience correcting the leprosy-affected nose. They examined their results and experience with over 17 leprosy patients. Using a variety of auricular and costal cartilage grafts, they found that reconstruction of the leprosy nose resulted in satisfactory appearance in almost all cases with autogenous cartilage. Importantly, they found resorption of some of the grafts over a period of time. One can speculate that resorption of costal cartilage in leprosy may be higher than that in standard cases due to poor mucosal blood supply in this subset of patients. In addition, if leprosy is still active, the destructive nature of leprosy can lead to continued destruction of autogenous cartilage.
Alloplastic materials are another viable option for reconstruction of the leprosy saddle-nose. These implants are easy to obtain and easy to use. However, these materials are not biologically incorporated into the host tissue and therefore carry the highest rates of infection, extrusion, and foreign body reaction of any graft material [24]. In a nose with preexisting chronic inflammation and damaged microvasculature, such as that found in leprosy, the use of an alloplastic material may reignite the inflammatory response that could result in rejection and injury to the viable soft tissue envelope. Additionally, these grafts primarily provide augmentation rather than structural support during rhinoplasty. In a recent review of the use of polytetrafluoroethylene (PTFE) in rhinoplasty by Godin et al, the authors found a graft infection rate of 3.2% and recommended that PTFE not be used in patients with septal perforations [25].
In our experience, autologous costal cartilage has proven to be the most reliable material for nasal framework reconstruction when septal cartilage is either unavailable or insufficient. Costal cartilage will supply the surgeon with ample amounts of cartilage to repair any major structural defect, and since it is an autologous graft, there is no host immune response. Therefore, the rates of graft rejection, infection, and extrusion are extremely low [16, 19]. One concern with autologous costal cartilage is the theoretical potential for graft resorption. Multiple studies have shown no evidence of resoprtion of costal cartilage grafts when correct surgical technique is used [17, 26]. Additionally, Menger et al used autologous costal cartilage to reconstruct the nasal dorsum in 17 patients with saddle-nose deformities caused by leprosy, and noted only 1 case of complete resorption of the graft after a 2-year follow-up [6]. One author (ARS) has used autogenous costal cartilage in over 85 cases, and has noted resorption in one case, after an infection to the nose in an immunocompromised patient. This author has not noted any cases of warping or extrusion during this time.
Another concern with autologous costal cartilage grafts is the potential for warping, which despite careful technique, continues to be the primary problem with the use of autologous rib cartilage [19]. Adams et al recently demonstrated that the warping characteristics of irradiated and nonirrradiated rib cartilage are similar, and recommended the use of IHRC only in cases where autologous cartilage is unavailable or the patient desires avoiding donor site incisions [27]. Meticulous carving techniques, the removal of all perichondrium, and adequate support of the graft are crucial in obtaining desirable results. Additionally, insertion of the graft may be delayed for at least 30 minutes to allow initial warping to occur.
The authors of this study advocate the use of the extended columellar strut rather than the use of a standard columellar strut. An extended columellar strut is used when the septum is missing and/or deficient. In this case the entire native septum was absent. One common mistake of surgeons using this technique is to make the columellar strut “too wide.” Unfortunately, when the columellar strut is excessively wide the columella will appear wide and often widen the infratip lobule, creating an unrefined look to the nose. One advantage of costal cartilage lies in its strength, obviating the need for excessively wide grafts.
Recreation of the nasal dorsum is a challenge for surgeons. Many surgeons incorporate large costal cartilage pieces onto the nasal dorsum, in an effort to rebuild the nose. However, for most patients with a saddle nose deformity, the collapse occurs within the cartilaginous portion of the nose. The authors advocate a more technically advanced approach to dorsal augmentation. Rather than excessive augmentation of the nasal bridge, less costal cartilage is placed on the bridge of the nose. In addition, the bony dorsum is gently rasped to accommodate a dorsal graft. Overall, the effort should be to build a natural dorsum, rather than adding excessive bulk to the nasal upper third.
CONCLUSION
Despite great advances in Leprosy remains a common granulamatous process within the world. The satisfactory treatment of the saddle nose created by leprosy can be accomplished by using autogenous cartilage. Additionally, careful technical execution and sound aesthetic judgment are critically important to reconstructing these challenging deformities.
REFERENCES
- Prevalence of Leprosy. World Health Organization 2008.
- Britton WJ, Lockwood DNJ. Leprosy. Lancet 2004; 363:1209-1219.
- Schwarz RJ, Macdonald M. A rational approach to nasal reconstruction in Leprosy. Plast Reconstr Surg 2003;114(4):876-882.
- Farina R. Total rhinoplasty for deformities following leprosy. Plast Reconstr Surg 1957;20(1):78-82.
- Anita NH, Pandya NJ. Surgical treatment of the nasal deformities of leprosy: a 16-year review. Plast Reconstr Surg 1977;60(5):768-777.
- Menger DJ, Fokkens WJ, Lohuis PJFM, Kingels KJ, Trenite GJN. Reconstructive surgery of the leprosy nose: a new approach. J Plast Reconstr Aesthetic Surg 2007;60:152-162.
- Fokkens WJ, Nolst Trenite GJ, Vinmond M, et al. The nose in leprosy: immunohistology of the nasal mucosa. Int J Lepr 1998;66(3):328-339.
- Chemotherapy of leprosy. Report of a WHO Study Group. World health Organ Tech Rep Ser 1994;847:1-24.
- WHO Expert Committee on Leprosy. World Health Organ Tech Rep Ser 1998;874:1-43.
- Report on third meeting of the WHO Technical Advisory Group on elimination of leprosy. Geneva: World Health Organization; 2002. Report No. WHO/CDS/CPE/CEE/2002.29.
- Tardy ME Jr, Schwartz M, Parras G. Saddle nose deformity: autogenous graft repair. Facial Plast Surg 1989;6(2):121-134.
- Romo T 3rd, Sclafini AP, Sabini P. Reconstruction of the major saddle nose deformity using composite allo-implants. Facial Plast Surg 1998;14(2):151-157.
- Thomassin JM, Paris J, Richard-Vitton T. Management and aesthetic results of support grafts in saddle nose surgery. Aesthetic Plast Surg 2001;25(5):332-337.
- Tovey FI. Reconstruction of the nose in leprosy patients. Lepr Rev 1965;36(4):215-220.
- Farina R. Total rhinoplasty for the destroyed nose. In F. McDowell and C. Enna (eds.), Surgical rehabilitation in leprosy. Baltimore, MD: Williams & Wilkins 1974:143-148.
- Cardenas-Camarena L, Guerrero MT. Use of cartilaginous autografts in nasal surgery: 8 years of experience. Plast Reconstr Surg 1999;103:1003-1014.
- Collawn SS, Fix J, Moore JR, Vasconez LO. Nasal cartilage grafts: more than a decade of experience. Plast Reconstr Surg 1997;100:1547-1552.
- Tardy ME, Denneny J, Fritsch MH. The versatile cartilage autograft in reconstruction of the nose and face. Laryngoscope 1985;95:523-533.
- Lovice DB, Mingrone MD, Toriumi DM. Grafts and implants in rhinoplasty and nasal reconstruction. Otolaryngol Clin N Amer 1999;32(1):113-141.
- Murakami CS, Cook TA, Guida RA. Nasal reconstruction with articulated irradiated rib cartilage. Arch Otolaryngol Head Neck Surg 1991;117:327-330.
- Welling RO, Maves MD, Schuller DE, Bardach J. Irradiated homologous cartilage grafts: long term results. Arch Otolaryngol Head Neck Surg 1988;114:291-295.
- Burke AJC, Wang TD, Cook TA. Irradiated homograft rib cartilage in facial reconstruction. Arch Facial Plast Surg 2004;6:334-341.
- Congdon D, Sherris DA, Specks U, McDonald T. Long-term follow-up of repair of external nasal deformities in patients with Wegener’s granulomatosis. Laryngoscope 2002;112(4):731-7.
- Porter JP. Grafts in rhinoplasty: alloplastic vs. autogenous. Arch Otolaryngol Head Neck Surg 2000;126(4):558-561.
- Godin MS, Waldman SR, Johnson CM. Nasal augmentation using Gore-tex®: a 10-year experience. Arch Facial Plast Surg 1999;1:118-121.
- Cakmak O, Ergin T. The versatile autogenous costal cartilage graft in septorhinoplasty. Arch Facial Plast Surg 2002;4(3):172-176.
- Adams WP Jr, Rohrich RJ, Gunter JP, Clark CP, Robinson JB Jr. The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg 1999;103(1):265-270.
FIGURE LEGENDS
Figure 1: (A,C, E, G) Preoperative Views in the Frontal, Lateral, Oblique, and Base respectively, demonstrating a severe saddle nose deformity. Note the relative absence of tip support, resulting in tip underprojection and bulbosity. On lateral view, deficient premaxillary projection is noted. (B, D, F, H) Postoperative Views at 1 year in the Frontal, Lateral, Oblique, and Base respectively. There is significant improvement in dorsal height and in projection of the nasal tip and premaxilla. Nasal length has been augmented, and refinement of the nasal tip has been achieved.
Figure 2: (A) grafts consisting of costal cartilage and perichondrium from the left seventh and eighth ribs immediately over harvest and (B) after carving prior to placement (dorsal onlay graft, above and columellar strut, bellow)
Figure 3: (A) Intraoperative view demonstrating standard open rhinoplasty approach. Note that the patient’s lower lateral cartilages have been spared by her infection with Mycobacterium leprae. (B) Placement of extended columellar strut using multiple, interrupted permanent sutures.
Figure 4: Schematic diagram demonstrating reconstruction of the Leprosy nose with costal cartilage. Costal perichondrium was placed superiorly for augmentation of patient’s radix (A). Dorsal augmentation was achieved by placement of two onlay grafts (B,C). Tip support was reestablished with an extended columellar strut (D), and the premaxilla was enhanced with multiple small pieces of costal cartilage.


