Defining the Facial extend of the Platysma Muscle
A Review of 71 Consecutive Face-lifts
Anil R. Shah, MD; David Rosenberg, MD
Objective: To delineate the superior (facial) extent of the platysma muscle.
Methods: A total of 142 facial halves were examined from 71 consecutive deep-plane rhytidectomies performed over a period of 3 months. The platysma muscle was identified and isolated during the procedure. The superior extent of the platysma was measured along the line created by the angle of the mandible to the malar eminence, also known as the malar mandibular line.
Results: On average, the platysma extended 3.98 cm along the malar mandibular line, superiorly from the inferior border of the mandible. The platysma was located 3.09 cm inferiorly from the malar eminence along the malar mandibular line. On average, the platysma muscle occupied 56% of the malar mandibular line.
Conclusion: The platysma muscle may have a more significant facial extension than previously described.
Arch Facial Plast Surg. 2009;11(6):405-408
DESPITE THE MYRIAD OF face-lift techniques available, few surgeons who perform face-lifts would question the role that the platysma muscle plays in rejuvenation of the aging neck.1 However, the extension of the platysma into the face has not been well described. Many anatomy textbooks depict the platysma muscle with its superior border limited by the inferior edge of the mandible (Figure 1). 2 However, we believe that the platysma muscle has a significant facial extension onto the face (Figure 2). One of us (D.R.) has developed a technique—a variant of deepplane rhytidectomy—in which the platysma muscle is isolated within the face and neck. Based on more than 7 years of experience with this technique and more than 1000 patients treated, the platysma muscle has been shown to constitute a critical component in the facial aging process. To support this theory, we performed a prospective anatomic study on 71 consecutive patients undergoing rhytidectomy.
During deep-plane rhytidectomy, a unique anatomic perspective exists when the dissection takes place along the undersurface of the platysma muscle (Figure 3 and Figure 4). When the masseteric fibers are released and separated, the extent of the platysma muscle can be clearly seen, based on the directional aspects of the muscle fibers and the often thick nature of the facial platysma. During surgery, attenuation of the facial platysma can be seen clearly at the midface along its superior extent.
The platysma muscle is a thin sheetlike muscle that originates on the fascia of the deltoid and pectoral regions and runs superiorly and medially, inserting on the mandible, the skin of the cheek, the commissure of the mouth, and the orbicularis oris muscle. 3 The only bony insertion of the muscle lies on the anterior third of the mandible. When the platysma muscle tenses, it lifts the neck out (accentuating platysmal bands) and lowers the eyelids and midface (accentuating the malar and nasolabial folds) and the mandible (making the neck shorter and wider), making it the major muscle responsible for the emotive response of surprise. Clinically, the actions created by the platysma clearly demonstrate a significant facial component.
Many of the mentioned findings associated with platysma muscle activity are seen with natural aging.4 With advancing age, the platysma tends to become thinner and less defined. 3 In addition, normal aging will cause the platysma muscle to sag and weaken, which creates un which creates unsightly platysmal bands or ptosis of the muscle and underlying tissues.

Figure 1. Artist’s depiction of the platysma muscle demonstrates the classical concept of the superior extent of the muscle limited to the inferior border of the mandible.
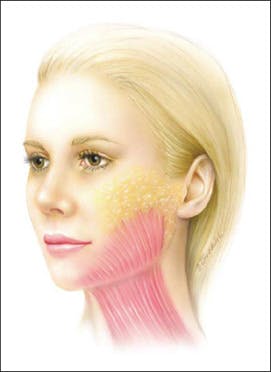
Figure 2. Artist’s depiction of the clinical superior extent of the platysma muscle attenuated near the midface.
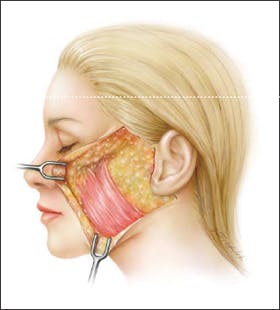
Figure 3. Artist’s depiction of the platysma muscle with a significant extent into the midface when the skin of the face is litled.
The platysma is the most superficial muscular layer of the face and is innervated by the cervical branch of the facial nerve. Embryologically, the platysma muscle is derived from the more superficially lying platysma fascia rather than the deeper-lying sphincter colli, in which the muscles of the face arise.5 Beneath the platysma muscle within the face lies an embryologic glide plane that separates the platysma muscle, derived from the second branchial arch, from the deeper-lying masseter, a derivative of the first branchial arch.
The goal of this study was to measure the superior extent of the facial platysma muscle. The implications and applications of our findings are briefly discussed.
METHODS
Based on more than 7 years of experience and more than 1000 patients in whom this technique has been used, we conducted a prospective study in which the anatomy of the platysma was analyzed in 71 consecutive deep-plane facelifts performed from October 1 through December 31, 2007. Patients included in this study underwent primary, revision, and multiple revision facelifts.
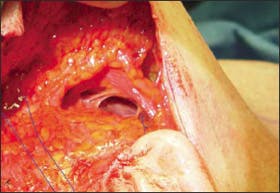
Figure 4. Intraoperative photograph shows the platysma in relation to the mandible and zygoma. Contrary to many anatomic descriptions, the platysma muscle will often have a thick muscular component in the face as shown.
All procedures in this study were performed by one of us (D.R.). The technique used is a unique variant of a deep-plane rhytidectomy, in which the platysma muscle is isolated and identified within the face and neck. To isolate the facial component of the platysma, a No. 10 blade scalpel is used to dissect the superficial musculoaponeurotic system (SMAS) laterally from the line created by the true zygomatic insertion point to the angle of the mandible. Dissection deep to the platysma muscle occurs approximately 1 cm posterior to the nasolabial fold along the face and 2 cm below the mandible. Oblique fibers of the platysma muscle are clearly seen on the undersurface of the dissection, distinguishing it from the underlying muscles in the face. The direction of the fibers of the platysma muscle distinguish it from other underlying muscles along the face.
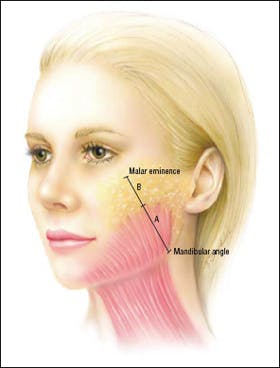
Figure 5. Artist’s depiction shows the measurements from the mandibular angle to the malar eminece, a line termed the malar mandibular line. Line A refers to the line created by the angle of the mandible to the superior extent of the platysma, whereas line B refers to the superiors extent of the platysma to the malar eminence.
For our study, the platysma muscle was measured along the line created by the angle of the mandible to the malar eminence, also known as the mandibular malar line (MML), by the same surgeon (D.R.). These landmarks were chosen in part because they were easily palpated and replicable from one patient to another. In addition, the fibers of the platysma muscle tend to parallel this line. The superior extent of the platysma muscle was measured from the inferior border of the angle of the mandible along the MML to the attenuation point of the platysma (Figure 5, line A). An additional measure was taken from the malar eminence to the superior border of the platysma along the MML, termed line B (Figure 5). The distance of the MML was calculated in every patient, because of the normal variance associated with face size.
RESULTS
Overall, 71 consecutive patients underwent deep-plane rhytidectomies in which the platysma muscle was measured. Sixty-four patients were women and 7 were men. Seventeen patients had undergone previous rhytidectomies, whereas 54 underwent primary face-lifts.
For all patients, the average distance of line A, the superior extent of the platysma muscle along the MML from the angle of the mandible, was found to be 3.98 cm. The average distance from the malar eminence to the superior border of the platysma muscle along the MML, line B, was 3.09 cm. The platysma muscle occupied 56% of the distance of the MML.
In the 7 male patients in the study, line A averaged 3.65 cm, whereas line B averaged 3.15 cm, occupying 54% of the face. Line A in the 64 female patients averaged 4.12 cm, whereas line B averaged 3.09 cm, occupying 57% of the face. When we compared male and female patients, we found that the distance was greater and that the facial platysma occupied a higher percentage of the face in female patients, although the difference was not statistically significant.
In the 17 patients undergoing revision face-lifts, line A averaged 3.27 cm, whereas line B averaged 3.04 cm, meaning that the platysma occupied 52% of the face. Fiftyfour patients underwent primary rhytidectomy, and lines A and B in these patients averaged 4.32 and 3.11 cm, respectively, with the platysma occupying 58% of the face. The facial platysma was found to be lower along the MML in patients undergoing revision compared with primary rhytidectomy.
COMMENT
This is, to our knowledge, the first study to formally determine the facial extent of the platysma. The traditional view of the platysma (see Figure 1) depicts a muscle that is mostly cervical in nature. However, our study demonstrates that the platysma muscle has a significant extension onto the face (see Figure 2).
There are several reasons why we believe that the facial component of the platysma has been underappreciated. Typically, anatomists use an outside-in approach when studying muscle layers. The intimate relationship between the overlying fascia and fibers of the platysma may obscure this relationship and make it difficult to use this approach. By using a natural embryologic glide plane during the procedure, the undersurface of the platysma muscle can readily be visualized (see Figure 3). In addition, facial rejuvenation has focused specifically on the SMAS. Although the SMAS clearly plays a role in facial rejuvenation, much of the credit given to the SMAS may in fact be owed to the facial platysma.
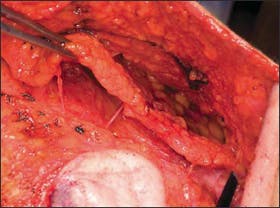
Figure 6. Operative photograph of the approach to facial rejuvenation in which the platysma muscle is isolated as a single unit in the face and the neck. The thick muscular component of the platysma muscle allows for a robust flap for rejuvenation of the face.
The SMAS is often considered an anatomic extension of the platysma. The SMAS is a fibrous fatty layer that was described as a distinct facial component in the landmark study by Mitz and Peyroine.6 We believe that distinguishing the SMAS from the platysma is important for several reasons. First, the face and neck should be thought of as a unified concept rather than separate components. When the SMAS and platysma are treated as 2 separate components, we have seen noticeable sagging along the jawline and an unnatural component, creating a visual disharmony along the face. Treating the face and neck as a single unit will allow for a more natural appearance (Figure 6). To keep the platysma muscle as a single unit and not attenuate its lateral fibers, we start the dissection laterally. In addition, in our experience, minimizing the subcutaneous elevation of the flap will lead to fewer postoperative vascular issues.
Other authors studying aspects of facial anatomy have noted the extent of the platysma in the face. Mendelson et al 7 recently described the anatomy of the jowl and noted the platysma muscle overlaying this area. When studying the anatomy of the midface, Gassner et al8 also noted that the platysma muscle was present within the face. We found that the platysma muscle was actually lower in the face in patients undergoing revision face-lifts compared with patients undergoing primary face-lifts. Deepplane rhytidectomy techniques were not used for the previous procedure for any of the patients who underwent a revision face-lift. A future study examining the location of the platysma muscle based on previous techniques may provide insight into the differences attributed to various rhytidectomy techniques and their role in repositioning the facial platysma. Because of the low numbers in this study, a definitive conclusion would not be advisable.
Our method of measuring the platysma muscle in a surgical setting should be noted. We wanted a method that could be easily replicated. In addition, the platysma muscle fibers extend across the face at an angle, rather than perpendicular to the Frankfort horizontal line. Clinical implications of this study demonstrate that the platysma muscle may change face and neck rejuvenation into a unified concept rather than dividing it into the 2 components of SMAS and platysma. In conclusion, our study supports the notion that the platysma muscle has a significant facial component. Further anatomic studies are necessary. The facial platysma muscle may play a larger role in surgical procedures on the aging face than previously thought.
REFERENCES
- Labbe’ D, Franco RG, Nicolas J. Platysma suspension and platysmaplasty during neck lift: anatomical study and analysis of 30 cases. Plast Reconstr Surg. 2006; 117(6):2001-2010.
- Moore KL, Agur AM. Essential Clinical Anatomy. Baltimore, MD: Williams & Wilkins; 1995.
- de Castro CC. The anatomy of the platysma muscle. Plast Reconstr Surg. 1980;66 (5):680-683.
- Kocer U, Ozdemir R, Ulusoy G, et al. Anatomy of the platysma muscle and the evaluation of it for the reconstruction of facial defects. J Craniofac Surg. 2005; 16(3):463-470.
- Keibel F, Mall FP. Manual of Human Embryology. Philadelphia, PA: Lippincott Williams & Wilkins; 1910:509-515. http://www.archive.org/details/manualhumanembr00mallgoog. Accessed October 15, 2008.
- Mitz V, Peyronie M. The superficial musculo-aponeurotic system (SMAS) in the parotid and cheek area. Plast Reconstr Surg. 1976;58(1):80-88.
- Mendelson BC, Freeman ME, Wu W, Huggins RJ. Surgical anatomy of the lower face: the premasseter space, the jowl, and the labiomandibular fold. Aesthetic Plast Surg. 2008;32(2):185-195.
- Gassner HG, Rafii A, Young A, Murakami C, Moe KS, Larrabee WF Jr. Surgical anatomy of the face: implications for modern face-lift techniques. Arch Facial Plast Surg. 2008;10(1):9-19.