Alar Base Resection and Repair Chicago Illinois
Introduction / Background
An overly wide or flared alar base will lead to a bottom heavy nose and disrupt the delicate balance of an otherwise properly executed rhinoplasty.
Classically, alar base refinement was thought to be necessary in only those alar bases that were wide pre-operatively. However, changes during rhinoplasty can affect the alar base width and the amount of alar flare. Several authors have noted that deprojection of the nasal tip will often lead to subsequent widening of the nostrils; 15% to 20% of deprojection rhinoplasties require wedge resections. (1-3) Placement of alar rim or contour grafts will reduce small amounts of alar retraction and improve nostril base triangularity at the expense of increased nasal base width. (4) Advancement of the maxillary base tends to widen the alar base complex. (5)
Anatomy

The alar base is a complex three dimensional shape, with intimate relationships with the medial cheek, nostril, columella, and upper lip.
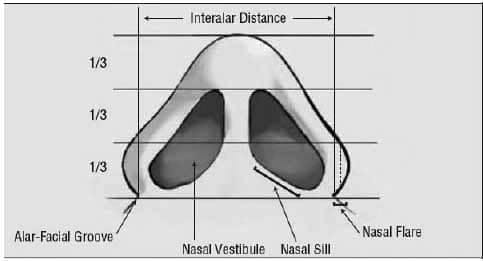
The appropriate terminology of the alar base is depicted in figure 1.
The alar base is typically composed of fibrofatty tissues and may assume a variety of shapes and sizes. The nasal sill, as defined by Tardy, refers to the intranostril region between the medial crural footplate/columella complex and the alar facial groove. (6) The nasal sill may be notched or smooth depending on the interface with the alar facial groove. The alar crease (alar facial groove) is the junction between the nose and cheek and is an important landmark to be preserved in rhinoplasty surgery. A cephalically positioned alar facial junction will lead to a snarled appearance to the nose, while a caudally positioned alar facial junction can lead to alar hooding. The columella or the feet of the medial crus comprises the most medial portion of the nostril and may significantly narrow the nostril aperture.
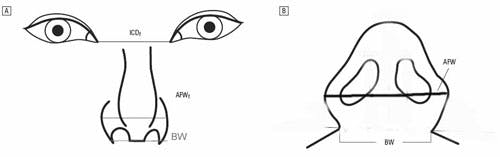
Lengths of several distances are calculated in order to individually optimize alar base reduction. The base width refers to the width of the nostril on base view at the alar facial junction. (see figure 2)
Read more about Dr. Shah’s Rhinoplasty Procedure for Alar Base Reduction here.
The flare width refers to the lateral aspect of the ala extending beyond the alar-facial groove, often the widest point of the nostril on base view. (7) These two components of analysis should be viewed as distinct aesthetic concerns. In addition, the shape and size of the nostril should be characterized. Sheen defined the alar axis which can be divergent, straight or convergent. (8) The internal length and external length of the alar sidewall should be measured and analyzed.
Preoperative Assessment
Preoperative counseling should examine how to harmoniously balance the patient’s aesthetic needs as related to ethnicity, facial characteristics, and patient treatment goals. Since the alar base varies considerably from person to person, a dogmatic approach and application of the classic canons of alar base aesthetic ideals will result in dissatisfied rhinoplasty patients. Divergent views by multiple authors upon the ideal aesthetic base support this viewpoint. Preoperative imaging is a useful tool in communicating between surgeon and patient. Computer photo imaging is an integral part of preoperative planning. It visually sets the esthetic goal for the patient and surgeon, and the nuances of alar width, alar flare, and nostril show can be completely discussed and defined.
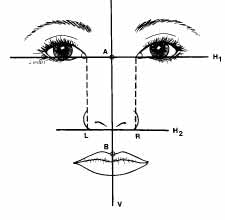 Classically the width of the alar base is thought to mirror the inner canthus. Guyuron contends that the ideal horizontal width of the alar base should be 1 mm wider than the inner canthus. (9) (See Diagram 3)
Classically the width of the alar base is thought to mirror the inner canthus. Guyuron contends that the ideal horizontal width of the alar base should be 1 mm wider than the inner canthus. (9) (See Diagram 3)
He also notes the ideal relationship of the alar facial junction is 2 mm caudal to the normally placed subnasale on lateral view. In ethnic noses, the patient’s treatment goals range from preserving the full width and flair of the alar base to narrowing of the nose to Western ideals. The width of the base should be analyzed not just in terms of intercanthal distance, but also of facial width and proportion.
Table 1 discusses the treatment options which can be utilized for each patient encounter.
- Treatment options (Adv/Disadv- Table)
- Wedge excision
- Sill excision
- Combination sill/wedge excision
- Base narrowing suture
- V-Y advancement (rare)
Wedge excisions improve excessive alar flare. These excisions will not narrow the nostril. They require an external incision.
Sill excisions narrow the alar base and nostrils. Sill excisions will not improve alar flair and occasionally may increase it. (See diagram 4)
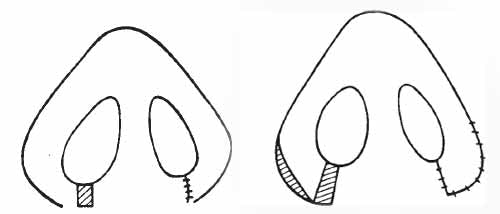
In fact, often after removal of excessive sill, the ratio of flair width to base width is accentuated, resulting in a need to remove excessive alar flare. Sill excisions in isolation are useful in patients with isolated alar base width and minimal to no flaring present.
The sill and wedge excision techniques are often combined into a combination sill/wedge technique, described by Adamson, among others. (10) This technique removes excess width in combination with flair. A calculated sill excision is combined with a wedge excision to narrow the nose where appropriate. Visible external incisions along the alar facial junction are a potential sequlae, but uncommon with meticulous technique.
Extremely wide nasal bases may require alternative or adjunctive treatment options. Base narrowing sutures are sutures placed across the length of the patient’s base width. When these sutures are tightened, the distance between the base width decreases. This technique does not create a visible incision and may result in increased nasal tip projection. The main drawbacks with this technique are difficulty in achieving long lasting results and prediction of final alar base position. V-Y advancement can be performed on wide nasal bases but must be tempered against the risk of placing a scar in a highly visible location. (11)
The location of the alar base excision should be thought of as either horizontal or vertical. The horizontal runs laterally across the sill and the vertical runs in the direction of the columella from the base to the nasal tip. If tissue is excised in a horizontal axis, the nasal base is narrowed but the ala will tend to flare more. Excision of tissue in the vertical axis shortens the alar rim and decreases the alar flare. The sill excision translates into horizontal excision. Appropriate location of the excision will reduce sill notching. The excision of tissue lateral to the alar facial groove will reduce flare and is also known as a wedge excision.
- Surgical Technique – Combination Wedge and Sill Technique
- Key instrumentation and materials
- 5-0 nylon suture with possible 5-0 PDS deep suture
- Sharp measuring calipers
- Ruler
- 11 blade
- Marking pen
- Bishop-Harmon
- Fine needle driver
- Frazier tip suction catheter, size 8
- Key instrumentation and materials
The nostrils are injected 15 minutes prior to the alar base reduction with a solution (1% lidocaine and 1:100,000 epinephrine) to allow adequate time for vasoconstriction to take place. Cautery is usually not necessary and should be avoided unless absolutely necessary. Hemostasis is achieved with closure. Excess cautery can lead to impaired wound healing and objectionable scarring. Sill and wedge excisions serve different purposes and can be performed as separate procedures, but are often combined due to patient anatomic needs.
Sill Excision
Sill excisions are performed for wide alar bases. At the completion of the rhinoplasty, the columellar midline at the nasolabial junction, the lateral-most points of the alar-facial groove, and the sill crease are marked. (Figure 5)
The side with the most alar flare is assessed for the amount of reduction necessary of the outer alar width and the inner nostril width. A ruler measures the distance from the crease point of the sill to the midline (usually 10-12 mm). The contralateral side is marked at the same distance so the resulting sill creases are bilaterally symmetric.
The nostril sill may dictate where a sill excision can be made. In most patients, there is a notch or crease where the sill meets the nostril. If the nostril sill’s junction with the nostril is smooth, sill reduction can take place anywhere along the sill. If the junction between the sill is notched, the sill incision should be placed in a flat location.
The desired amount of narrowing of the outer diameter of the ala is determined and calipers are used to sharply stab the skin from the desired sill crease to the ala. Medial and then lateral sill incisions are made with a no. 11 blade cutting upward from the stab. (Figures 6 and 7)
The starting point of the lateral cut will determine the outside nostril diameter, while the angle of cut into the nasal vestibule determines the ultimate inner nostril diameter. The amount and location of the nostril resected will lead to reduction in either nostril size or alar base size. (Figure 8).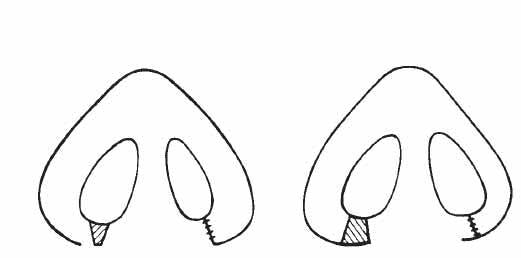
The shape applied to the alar base reduction will affect the alar base as well. The nostril should be thought of as with an internal circumference and an external circumference. Reduction of the internal circumference will diminish nostril size. Reduction of the external circumference will narrow the alar lobule. The surgeon can therefore tailor the amount of nostril reduction and alar base reduction to each individual patient.
The caudal extent of both incisions is then connected with a no. 11 blade along a line that begins medially parallel to the sill and travels to the lateral alar-facial mark. Care is taken to stay just above the actual alar-facial crease, preserving the actual crease instead of cutting into it. The incision should be placed 1 mm above the alar facial junction. Any incision placed within the crease may lead to suture marks or distortion of the alar facial junction.
The sill is approximated with a medial 5-0 nylon tacking suture. If a wedge excision is to be performed in addition, this will be performed next. If a sill excision is to be performed by itself, interrupted 5-0 nylon sutures are used to close the incision. In patients with large amounts of sill excised, a deep suture can be placed to alleviate any wound tension on the incision.
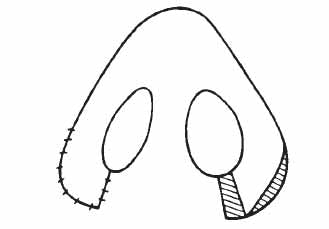
Wedge Excision in Combination with Sill Excision
Sill excisions may accentuate the relative amount of alar flaring. In those patients, wedge excisions should be combined with sill excisions. To estimate the required amount of alar flare reduction, the incised alar lobule is grasped at its caudal cut edge with a Brown-adson forceps and pulled inferiorly. (Figure 9) A no. 11 blade is used to excise this wedge of tissue. A tacking suture is placed at the midline of the reconstituted ala. If more ala narrowing is desired, the medial tacking suture is removed and additional alar tissue is resected. The wound is closed meticulously with 5-0 nylon suture in an interrupted fashion.
Wedge Excision in Isolation
A wedge excision can be made in isolation for isolated alar flair. The incision is typically made 1 mm anterior to the alar facial junction. A calculated wedge of nostril is removed. Some authors have noticed improved scarring with preservation of the underlying muscle with this technique. (1) The incision is made with a number 11 blade and tissue is handled delicately with a bishop tissue forceps. The wound can be closed in multiple layers with 4-0 suture placed deep and the epidermis closed with either 5-0 or 6-0 nylon suture in an interrupted fashion.
Postoperative Care
Alar base incisions will tend to crust if not cared for appropriately. The patient applies antibiotic ointment to the wound immediately after the procedure three times a day. Patients are given hydrogen peroxide solution and instructed to gently clean any crusts forming on the sutures. Patients are seen on postoperative day number one and incisions are inspected, all crusts are debrided and antibiotic ointment is applied.
Typically, sutures are removed from the wedge excision on postoperative day five. However, consider removal at day seven or eight if wound healing is not sufficient. Steristrips can be used to reinforce the wound to assist healing. Sutures along the sill may be left in place for up to two weeks.
Complications and their management
Overall, most patients are satisfied with alar base narrowing. However, there are some complications which can occur. Unsightly scarring or notching is rare if meticulous closure techniques are adhered to. Scars which are visible can be dermabraded at 8 weeks or re-excised at a later date
Achieving perfectly symmetric nostrils with preexisting nostril asymmetries is nearly impossible. Cinelli describes a technique described to minimize postoperative asymmetry called the “Calibrated Weir Operation”. (12) It involves drawing a midcolumellar line from the nasolabial angle to the midpoint of the upper vermillion border, then bisecting this line and the columella with another perpendicular line. From the intersection of the 2 lines, one may measure the distance to the medial and lateral borders of a nasal base excision. Similarly, the senior author has found precise identification of the midcolumella and lateral starting point of the nasal sill with calibrated precise removal of tissue has resulted in excellent surgical postoperative symmetrical results. (7)
Nostril stenosis is a surgical error of commission and can be avoided by conservative and appropriate narrowing. Surgical correction of overly narrowed nostrils is difficult and can involve a composite flap, local flap, and/or stent placement. (13) Additionally, loss of alar crease is often the result of poor incision planning. This natural border is very difficult to recreate surgically and requires recruitment of tissue laterally.
Tear drop or Q deformity may result from overly aggressive excisions of the lateral alar wall. (1) However, Toriumi has noted that meticulous closure has minimized this deformity and hidden resultant scars satisfactorily. (4)
Future Considerations
Alar base reduction has not changed significantly in the last 20 years of rhinoplasty. Areas which are current challenges are augmentation of the alar base. Alar bases at different insertion points may require cartilage grafting to change the height of the alar base. In addition, alar bases which are excessively narrowed may require techniques which are not yet established to widen and provide an adequate airway and natural contour to the nostril.
Read more about Dr. Shah’s Rhinoplasty Procedure for Alar Base Reduction here
References
- Kridel RW, Castellano RD. A Simplified Approach to Alar Base Reduction: A Review of 124 patients over 20 Years. Arch Facial Plast Surg. 2005;7:81-93.
- Rees TD. Aesthetic Plastic Surgery. Philadelphia, Pa: WB Saunders Co; 1980:243-273.
- Gilbert SE. Alar Reductions in Rhinoplasty. Arch Otolaryngol Head Neck Surg. 1996;781-784.
- Toriumi DM. New Concepts in Nasal Tip Contouring. Arch Facial Plast Surg. 2006;8:156-185.
- Guyuron B. Dynamics of Rhinoplasty. Aesthetic Plast Surg 2002;26 Suppl 1:10.
- Tardy ME, Patt BS, Walter MA. Alar reduction and sculpture: anatomic concepts. Facial Plast Surg. 1993;9:295-305.
- Bennett GH, Lessow A, Song P, Constantinides M. The Long-term effects of alar base reduction. Arch Facial Plast Surg. 2005;7:94-97.
- Sheen JH. Aesthetic Rhinoplasty. St. Louis, Mo: CV Mosby Co, 1978.
- Guyuron B, Behmand RA. Alar base abnormalities. Classification and correction. Clin Plast Surg. 1996;23(2):263-70.
- Adamson PA, Oakley S, Tropper GJ, McGraw BL. Analysis of alar base narrowing. Am J Cosmet Surg. 1990;7:239-243.
- Bernstein L. Rhinoplasty for the Negroid nose. Otolaryngol Clin North Am. 1975: 8:785-795.
- Cinelli JA. Calibrated Weir operation. Arch Otolaryngol. 1961;74:189-191
- Egan KK, Kim DW. A novel intranasal stent for functional rhinoplasty and nostril stenosis. Laryngoscope. 2005;115(5):903-9.
Figure Legends
Figure 1: The alar facial groove is the location of the alar base insertion point on the face. The nasal sill is located between the medial crus/footplate complex and the alar facial groove.
Figure 2. The base width (BW) refers to the width of the nostril on base view at the alar facial junction. The flare width (FW) refers to the lateral aspect of the ala extending beyond the alar-facial groove, often the widest point of the nostril on base view
Figure 3. According to Guyuron, the ideal horizontal width of the alar base should be 1 mm wider than the inner canthus.
Figure 4. When a sill excision is performed, the alar base is effectively narrowed. The ratio of the alar flair to alar base has now increased, leading to a relative increase in alar flair. When a sill excision is executed in conjunction with a wedge excision, the ratio of alar flair to alar base is reduced, leading to an improved aesthetic.
Figure 5. Markings are place in the columella midline, in the lateral most points of the alar-facial grooves, and in the crease equidistant from the midline. The desired narrowing of the outer diameter of the ala is determined and marked with calipers.
Figure 6. Sill incisions are performed with a no. 11 blade cutting upward from the stab. The starting point of the lateral cut will determine the outside nostril diameter, while the endpoint in the nasal vestibule determines the ultimate inner nostril diameter.
Figure 7. The caudal extent of both excisions is connected with a no. 11 blade along a line that begins medially parallel to the sill and travels to the lateral alar-facial mark.
Figure 8. The amount and location of the nostril resected will lead to reduction in either nostril size or alar base size.
Figure 9. After the sill is tacked medially, the alar lobule is grasped with a Brown-Adson forceps and pulled inferiorly to estimate the amount of alar flare reduction. A no. 11 blade is used to excise the wedge of tissue.
“The nose should fit the face”
A strong jawline would suggest a stronger nose.